How Strength Training Can Help Resolve Stress Urinary Incontinence

By Dr. Norah Whitten
Role of Strength Training in Resolving Stress Urinary Incontinence
If you experience bladder leakage when you sneeze, laugh, jump, or lift something heavy, you’re not alone. Stress urinary incontinence (SUI) affects millions of people, especially women, and it can significantly impact daily life, confidence, and participation in fitness.
But here’s the good news: strength training, when done strategically and safely, can play a powerful role in reducing and even resolving symptoms of stress incontinence.
What Exactly Is Stress Urinary Incontinence?
Stress urinary incontinence is the involuntary leakage of urine during activities that increase pressure in the abdomen like coughing, laughing, jumping, or running. It’s most common among women, particularly those who have given birth, gone through menopause, or experienced pelvic floor trauma. However, SUI can affect people of all genders and fitness levels.
Contrary to popular belief, SUI isn’t always caused by a “weak bladder.” Instead, it often results from a lack of support from the pelvic floor and surrounding muscles that help manage intra-abdominal pressure during movement. This is why taking a whole body approach can be so effective!
While Kegels can help some people activate and become aware of their pelvic floor, they’re not always enough and sometimes they can even make things worse... Working with a pelvic floor physical or occupational therapist can help you determine what type of pelvic floor training is best for your body.
Dr. Norah Whitten
Why Strength Training Matters for Pelvic Health
When done with proper form and intention, strength training can help:
1. Improve Pelvic Floor Coordination
Rather than focusing solely on isolated pelvic floor contractions (like Kegels), full-body strength training helps the pelvic floor work in synergy with the diaphragm, deep core, and hips. This improves the timing and coordination needed to support the bladder during high-impact activities.
2. Enhance Core Stability
The core is more than just absit’s a system of muscles that includes the pelvic floor, diaphragm, transversus abdominis (the deepest abdominal muscle), and multifidus (a muscle in our back). Strength training that targets these areas helps create a stable base for movement and prevents excessive pressure from bearing down on the bladder.
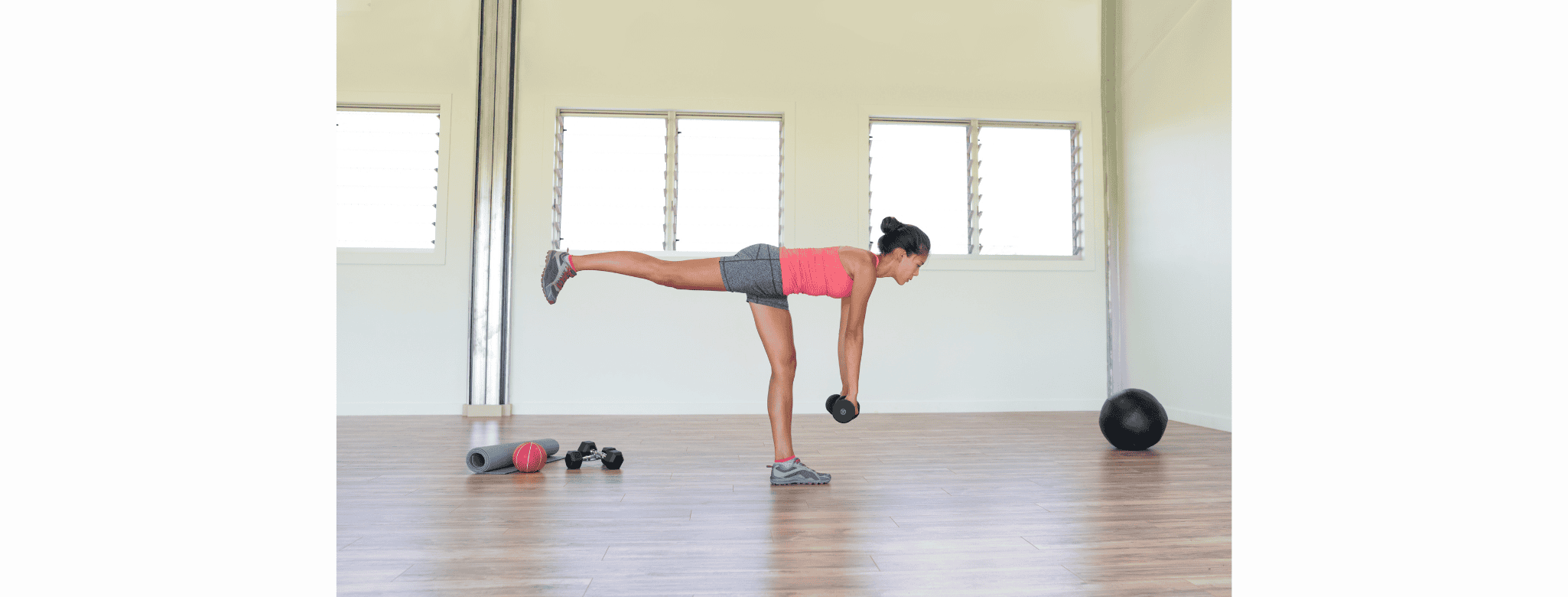
3. Build Strength and Function in Key Muscle Groups
Glutes, hips, hamstrings, and even lats play a role in pelvic alignment and pressure management. A well-rounded strength program reinforces the postural and muscular support needed to minimize leakage during everyday tasks and workouts.
4. Promote Better Posture and Breathing Mechanics
Many people with SUI have suboptimal posture or poor breathing patterns that increase downward pressure on the pelvic floor. Strength training, especially when incorporating breathwork and alignment awareness, can help retrain these habits for more effective bladder control.
Strength Training vs. Kegels: Why You Need Both (But Not Just One)
While Kegels can help some people activate and become aware of their pelvic floor, they’re not always enough and sometimes they can even make things worse.
Here’s why:
- Over-reliance on isolated exercises doesn’t teach your body how to use the pelvic floor functionally during movement.
- Some people with SUI actually have pelvic floor tension or coordination issues not weakness. In these cases, more Kegels may lead to more dysfunction.
- Full-body, progressive strength training builds the neuromuscular control and resilience you need to move leak-free through daily life.
Working with a pelvic floor physical or occupational therapist can help you determine what type of pelvic floor training is best for your body.
What a Bladder-Friendly Strength Routine Looks Like
Not all workouts are created equal when it comes to pelvic health. Here are some foundational principles for creating an SUI-safe strength routine:
✅ Focus on Form and Alignment
Maintaining a neutral spine, stacked ribcage, and aligned pelvis helps distribute pressure more evenly. Avoid breath-holding or excessive bracing.
✅ Coordinate Breath with Movement
Exhale during exertion (like the lift or push phase of an exercise) to reduce intra-abdominal pressure. Practice syncing breath with effort.
✅ Start with Low Impact and Build Gradually
Exercises like glute bridges, bird-dogs, squats to a box, and deadlifts with light weights are excellent starting points. Progress slowly to avoid pressure spikes that challenge bladder control too soon.
✅ Don’t Ignore the Glutes and Hips
Strong hips and glutes contribute to better pelvic alignment and support. Include exercises like clamshells, step-ups, and band walks.
✅ Include Core Stability Work
Instead of crunches, focus on anti-rotation and anti-extension core work like dead bugs, planks (as tolerated), and farmer’s carries.
Who Should Avoid Certain Exercises?
If you currently experience stress incontinence, avoid exercises that:
- Cause noticeable leakage
- Require breath-holding or straining
- Involve high-impact jumping or running (at least temporarily)
A pelvic floor therapist or personal trainer with pelvic health training can help you modify or progress exercises appropriately.
The Bottom Line: Strength Training Is Pelvic Health Training
Stress urinary incontinence is not something you have to just live with or avoid activities because of. With the right approach, strength training can be a game-changing tool for bladder control, core strength, and confidence.
If you’re unsure where to start, consult a pelvic floor physical or occupational therapist who can tailor a program to your body, symptoms, and goals.
About Dr. Norah Whitten. Dr. Norah is not only a physical therapist, but also an athlete, coach and mom. Norah utilizes the movement patterns and philosophies of functional fitness to get her patients the outcomes they deserve and help them become stronger than they ever thought possible. Dr. Norah attended the University of Illinois for her undergraduate work and Duke University for her Doctor of Physical Therapy. Since graduating from school Norah has specialized in working with an active population. She specifically got interested in treating the pelvic floor after noticing a gap in care for active pregnant & postpartum women.
Spread the word
Medical Disclaimer: All content found on the HER Health Collective Website was created for informational purposes only and are the opinions of the HER Health Collective experts and professional contributors. The Content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health providers with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this Website. If you think you may have a medical emergency, call your doctor, go to the emergency department, or call 911 immediately.